Creating an integrated programme to build confidence in primary care to manage axial SpA patients
Blog by Professor Antoni Chan, Consultant Rheumatologist and Associate Medical Director, Royal Berkshire NHS Foundation Trust.
Background
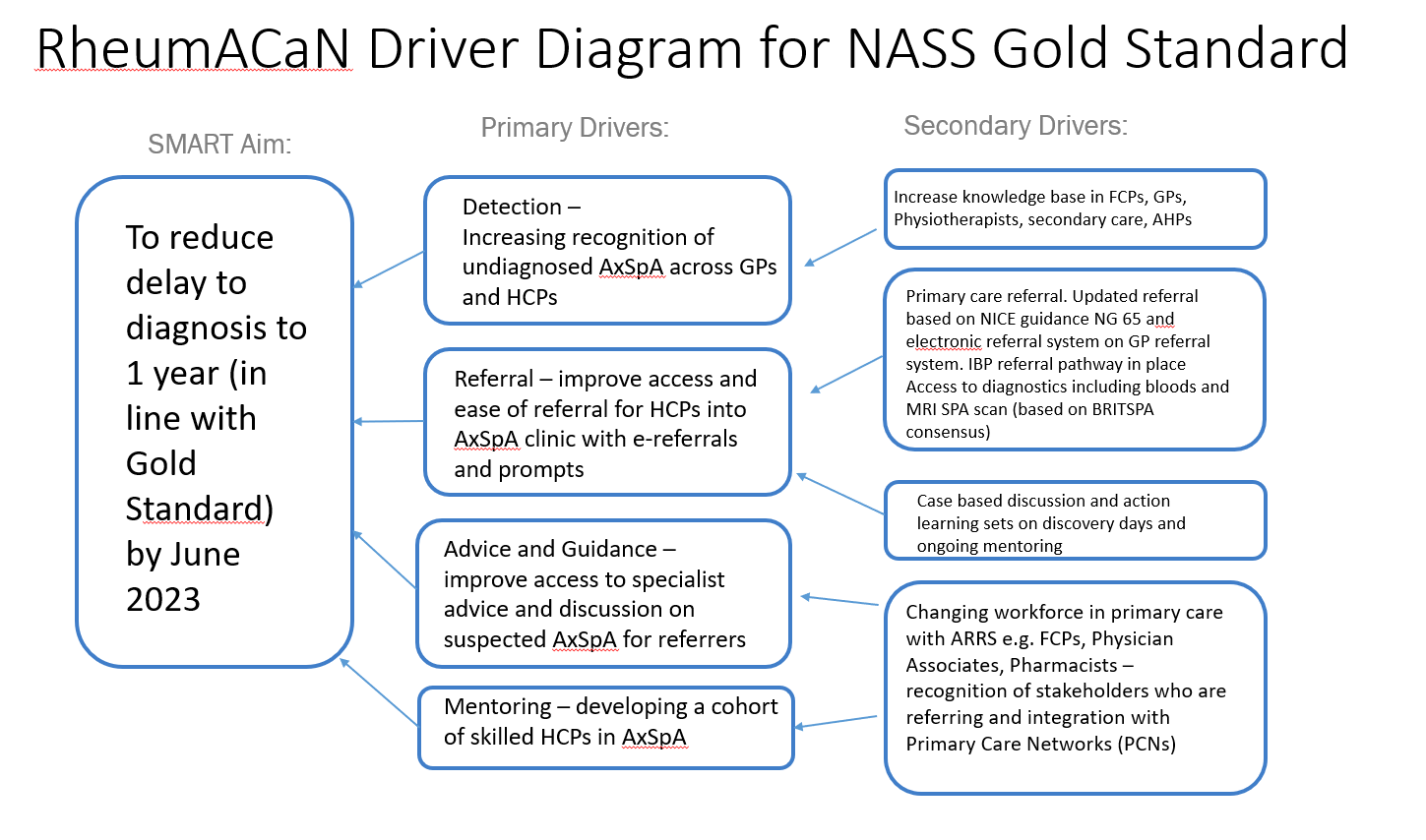
Improving the delay to diagnosis in axial spondyloarthritis remains an important challenge in rheumatology. In order to achieve this as well as improve the quality of referrals, we have created an integrated Rheumatology Academy and Collaborative Network (RheumACaN) for clinicians in primary care. RheumACaN aimed to build confidence in primary care to refer and manage patients with axial spondyloarthritis as well as other rheumatic diseases. Through the integration of pathways from primary to secondary care, RheumACaN aimed to reduce delays to diagnosis, improve referral from primary care and enhance management of patients.
You can listen to our Rheum for Improvement podcast, episode two, where Professor Chan discusses his teams project to improve access to mental health resources for patients with axial SpA and how they used data to drive their success.
How did you start the process of engaging patients?
We were conscious that there was a high number of patients with axial spondyloarthritis not engaging with physiotherapy. Patients were referred for physiotherapy through the spinal clinics by the Consultant, Nurse Specialist and Pharmacist, but many were either not attending their appointment or not opting in to get an appointment.
We had a vision of how we would like it to be and hoped that this would facilitate better engagement. We decided to change the process and involve physiotherapy from the beginning by being present at the clinic for the patient’s initial appointment. We also changed from using an opt-in appointment letter that relied on the patient contacting us to our receptionist phoning and offering a physiotherapy appointment. We developed a virtual spinal multidisciplinary team meeting to discuss newly diagnosed patients 4 months after diagnosis as well as complex patients. We used this to assess their progress and engagement and decide on what was the most appropriate review considering what was important to them.
What tactics did you use to engage your patients?
We put into practice the quality improvement skills we gained from Aspiring to Excellence. We focused on Solution 2 of the Gold Standard for Diagnosis which is to ensure swift identification of potential axial SpA in primary care. We measured our baseline, used driver diagrams and implemented PDSA cycles. RheumACaN is a 3-year rolling programme with face-to-face discovery day meetings sharing best practice, teaching and discussion on local referral pathways, guidelines and investigations. In between the face-to-face sessions, there was active learning through virtual mentoring. Participants completed action learning sets, case discussions and the course workbook. The outcome was measured through key metrics, referral patterns and feedback from participants.
What barriers (if any) did you face while working on your project?
We spent 9 months from the start of 2021 planning this programme. Engagement was key and we spent time getting feedback from GPs, physios, FCPs on what their learning needs were. This allowed us to shape our teaching materials including the workbook. We had workshops with the faculty to discuss the content before starting. We had regular coaching sessions with the NHS Transformation Team through Aspiring to Excellence for feedback. We also applied for funding for the programme.
Were there any light bulb moments? Or big wins?
Our big wins were that we had a train-the-trainer model. Participants in Cohort 1 came back to share and teach Cohort 2. Cohort 1 graduates have also been doing peer to peer teaching sessions in their own practices to help spread and ensure sustainability. This continuous loop of learning, mentoring and peer support makes this a unique programme, with a long-lasting impact far beyond that of a webinar, e-learning course or seminar, with knowledge which is tested and refined through a local lens. Our collective understanding of how to disseminate and implement best practices across diverse disciplines resulted in the rapid increase of early referrals of inflammatory arthritis from primary care in our centre which is now above the national average in the UK.
What was the result of your project? Is it still a work in progress or do you have outcomes you can share at this time?
RheumACaN was attended by 80 participants over 2 cohorts in 2021-2022. Prior to RheumACaN, the number and percentage of patients with suspected early inflammatory arthritis (EIA) referred to a specialist clinic within three working days which is a measure of primary care performance was 109/312 (32%) in 2018/19, 190/334 (57%) in 2019/20, 45/86 (52%) in 2020/21. Post RheumACaN, this increased to 140/201 (70%) in 2021/22. The national average for this metric was 47% in 2019/20 and 54% in 2021/22. We have developed an electronic referral system for GPs for suspected AxSpA. In AxSpa, the delays in diagnosis has reduced from a mean of 4.4 years from the onset of symptoms of back pain to a mean of 1 year in 2022. Feedback from 2 cohorts was 100% scored 5/5 (excellent) for how well the purpose of the programme was communicated, 100% scored 5/5 for how organised and easy to follow the programme was, 98% scored 5/5 for how engaged the presenters were. All participants responded that they had learned from the programme and this would change their practice. Narrative feedback included: “Very interesting – diagnosis and management, and when to refer onwards, very clear”, “Really helpful for future referrals, good tips what to look out for”, “Clear criteria and management (onward referral)”, “Enjoy discussing the cases and getting feedback, useful to hear other cases”, “Has given me a completely new way at looking at suspected axial spondyloarthritis”, “Can’t wait to see and refer a patient with suspected axial spondyloarthritis”.
Further information:
https://www.rheumatology.org.uk/news/details/Bridging-the-gap-between-primary-and-secondary-care
You can listen to our Rheum for Improvement podcast, episode two, where Dr Chan discusses his teams project to improve access to mental health resources for patients with axial SpA and how they used data to drive their success.